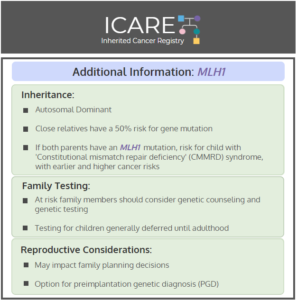
Gene: MLH1 Cancer Risks and Management (per NCCN version 3.2019): Women: Endometrial cancer risk: Elevated at 43%-57% – Consider risk-reducing hysterectomy. Ovarian cancer risk: Elevated at 5%-20% – Recommend risk-reducing bilateral salpingo-oophorectomy (removal of ovaries and fallopian tubes). Breast cancer risk: Elevated at 12%-17% – Manage same as general population. Men and Women: Colorectal cancer …
Syndrome: Constitutional Mismatch Repair Deficiency
Permanent link to this article: https://inheritedcancer.net/post3320/
ICARE Newsletter Winter 2017
The Potential Promise of Immunotherapy Targeted to Those with Bi-Allelic Mutations in Lynch Syndrome Genes
ICARE Newsletter Winter 2017
The Potential Promise of Immunotherapy Targeted to Those with Bi-Allelic Mutations in Lynch Syndrome Genes
People with Lynch Syndrome have a non-working Lynch gene (“mutation”), while the other copy of that gene is normal (recognizing that all of these genes come in pairs, with one member of the pair coming from each parent). Over the last few years, there has been an increased realization that some individuals have a mutation …
Permanent link to this article: https://inheritedcancer.net/2nlw2017/