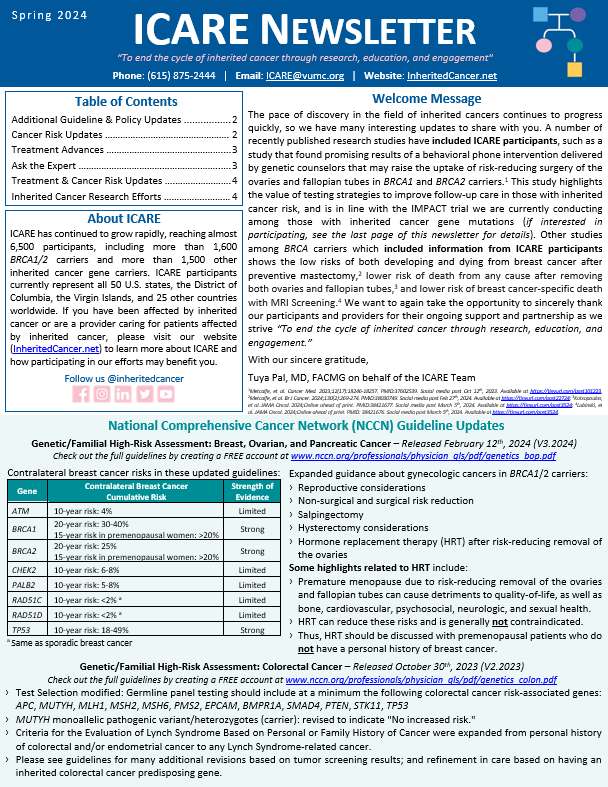
In January 2024, the American Society of Clinical Oncology (ASCO) in conjunction with the Society of Surgical Oncology released new guidelines for germline testing in patients with breast cancer, which include the following: For a full list of recommendations in this guideline, the article is available at: https://ascopubs.org/doi/10.1200/JCO.23.02225 Bedrosian, et al. J Clin Oncol. 2024;42(5):584-604. PMID:38175972. Social …
Tag: Genetic Test Interpretation
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2024-new-guidelines-released-through-asco-society-of-oncology-germline-testing-in-patients-with-breast-center/
ICARE Newsletter Fall 2023
Newly released ACMG Clinical Practice Resource on CHEK2 Developed Through a Group of Worldwide Experts!
ICARE Newsletter Fall 2023
Newly released ACMG Clinical Practice Resource on CHEK2 Developed Through a Group of Worldwide Experts!
A person with a pathogenic variant in the CHEK2 gene may be at an increased risk for developing breast and other cancers. This ACMG Clinical Practice Resource, published in ACMG’s flagship journal, Genetics in Medicine, provides valuable information for healthcare providers caring for individuals with pathogenic variants in the CHEK2gene. This new ACMG Practice Resource …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2023-newly-released-acmg-clinical-practice-resource-on-chek2-developed-through-a-group-of-worldwide-experts/
ICARE Featured Video November 2022
RAD51C Variants of Uncertain Significance
ICARE Featured Video November 2022
RAD51C Variants of Uncertain Significance
Below you may watch a featured video from the November 2022 Genetics Case Conference, which focused on RAD51C variants of uncertain significance with guest experts David Adams, PhD from the Wellcome Sanger Institute.
Permanent link to this article: https://inheritedcancer.net/video111022/
Permanent link to this article: https://inheritedcancer.net/post62221/
ICARE Social Media Post April 2021
Winter 2021 Ask the Expert
ICARE Social Media Post April 2021
Winter 2021 Ask the Expert
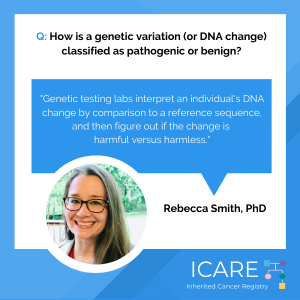
In every ICARE newsletter we give our participants the opportunity to have a question addressed by an expert in the field. In the latest edition, Dr. Rebecca Smith explains how a genetic change (or mutation) is classified as pathogenic or benign. Check out Dr. Smith’s full response in our Winter 2021 newsletter at: https://inheritedcancer.net/newsletters/
Permanent link to this article: https://inheritedcancer.net/post40921/
ICARE Newsletter Winter 2021
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
ICARE Newsletter Winter 2021
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
An old study back in 1999 suggested that CHEK2 may be a Li-Fraumeni Syndrome gene.1 However, a subsequent report in 2002 clearly refuted this original assertion, and based on additional data and analysis concluded that “… it is very unlikely that CHEK2 is an alternative Li-Fraumeni Syndrome susceptibility gene.”2 Another subsequent report in 2008 based …
Permanent link to this article: https://inheritedcancer.net/4nlw2021/
ICARE Newsletter Winter 2021
Ask the Expert
ICARE Newsletter Winter 2021
Ask the Expert
In each newsletter, we give participants the opportunity to have their questions addressed by experts in the field. This question was addressed by Rebecca Smith, PhD, Laboratory Director at Genetics Associates, Inc. with over 20 years of experience in biomedical research and 7 years of experience in clinical laboratory diagnostics. If you have a question …
Permanent link to this article: https://inheritedcancer.net/9nlw2021/
ICARE Social Media Post December 2020
CDH1 Cancer Risks
ICARE Social Media Post December 2020
CDH1 Cancer Risks
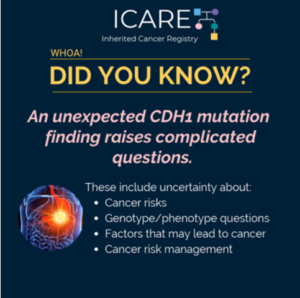
When a 𝘾𝘿𝙃1 mutation is identified, several factors should be considered to figure out what the cancer risks might be and what medical management should be advised. Specifically, differences in cancer risks among those with a 𝘾𝘿𝙃1 mutation are not well understood. Identifying a 𝘾𝘿𝙃1 mutation in families with hereditary diffuse gastric cancer (HDGC) …
Permanent link to this article: https://inheritedcancer.net/post121520/
ICARE Featured Video November 2020
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
ICARE Featured Video November 2020
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
Below you may watch a featured video from the November 2020 Genetics Case Conference, which outlined how CHEK2 is NOT a Li-Fraumeni Syndrome gene. For additional details, read the articles at the links below: 𝟭𝟵𝟵𝟵: https://pubmed.ncbi.nlm.nih.gov/10617473 𝟮𝟬𝟬𝟮: https://pubmed.ncbi.nlm.nih.gov/12442270 𝟮𝟬𝟬𝟴: https://pubmed.ncbi.nlm.nih.gov/18178638
Permanent link to this article: https://inheritedcancer.net/video111220/
ICARE Newsletter Summer 2020
Ask the Expert
ICARE Newsletter Summer 2020
Ask the Expert
In each newsletter, we give participants the opportunity to have their questions addressed by experts in the field. This question was addressed by Georgia Wiesner, MD, MS, a nationally renowned clinical cancer geneticist, who is an Ingram Professor of Cancer Research, Professor of Medicine in the Division of Genetic Medicine, and the Director of the …
Permanent link to this article: https://inheritedcancer.net/6nls2020/
Permanent link to this article: https://inheritedcancer.net/video51420/
ICARE Newsletter Summer 2019
Ask the Expert
ICARE Newsletter Summer 2019
Ask the Expert
The following question was addressed by Gillian Hooker, PhD, ScM, LCGC, who is the president-elect for the National Society of Genetic Counselors, Adjunct Associate Professor in the Division of Genetic Medicine at the Vanderbilt University Medical Center, and the Vice President of Clinical Development for Concert Genetics in Nashville, TN. Q. Why was the BRCA1/2 …
Permanent link to this article: https://inheritedcancer.net/10nls2019/
ICARE Newsletter Winter 2019
Testing Interpretation and Variant Reclassification
ICARE Newsletter Winter 2019
Testing Interpretation and Variant Reclassification
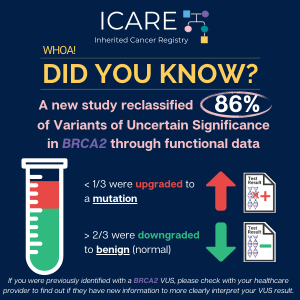
Results of germline genetic testing generally yield three types of test results: Deleterious (positive), Negative (no mutation detected), and Variant of Uncertain Significance (VUS). As more genes are tested, the chance for a positive result goes up, as does the chance of receiving a VUS result.1 VUS results tell us that it remains uncertain whether …
Permanent link to this article: https://inheritedcancer.net/15nlw2019/
ICARE Newsletter Summer 2011
Ask the Expert
ICARE Newsletter Summer 2011
Ask the Expert
We are fortunate to have Dr. Alvaro Monteiro, who is a molecular geneticist and expert on the BRCA1 and BRCA2 genes, as a member of our team. For our first ICARE newsletter, Dr. Monteiro teaches us about Variants of Uncertain Significance. Q. What is a Variant of Uncertain Significance (VUS) test result? How do researchers …
Permanent link to this article: https://inheritedcancer.net/1nls2011/