We recently published a study that brings attention to “reduced penetrance” BRCA1 and BRCA2 (BRCA) mutations, which lead to LOWER breast cancer risks than “typical” BRCA mutations.1 Specifically, these mutations lead to a lifetime breast cancer risk of 20-30%, similar to moderate penetrance breast cancer genes such as CHEK2 or ATM. This level of risk …
Tag: Variant of Uncertain Significance
Permanent link to this article: https://inheritedcancer.net/5nls2025/
ICARE Social Media Post January 2025
VUS Pilot Study Recruitment Post
ICARE Social Media Post January 2025
VUS Pilot Study Recruitment Post
📣 Are you or someone you know living with a Variant of Uncertain Significance (VUS) in an inherited cancer gene? We’re inviting you to enroll into ICARE to be considered for a valuable research effort focused on improving resources for those with a VUS result. When you participate in ICARE, you’ll:✔️ Be considered for this …
Permanent link to this article: https://inheritedcancer.net/post10425/
ICARE Social Media Post December 2024
RAD51C VUS Results
ICARE Social Media Post December 2024
RAD51C VUS Results
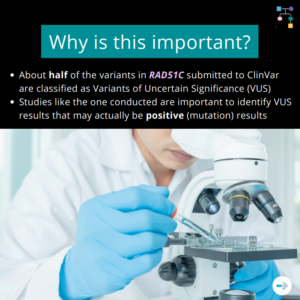
🔬A new study uses additional laboratory analyses to figure out which Variant of Uncertain Significance (VUS) results may actually be mutations (i.e., positive results): 📈 Why is this important? Read the full article to learn more at: https://www.sciencedirect.com/science/article/pii/S0092867424009681 Reference: Olvera-León, et al. Cell. 2024;187(20):5719-5734.e19. PMID: 39299233.
Permanent link to this article: https://inheritedcancer.net/post122324/
ICARE Social Media Post June 2023
VUS Results: Rates of Reclassification in Inherited Cancer Genes
ICARE Social Media Post June 2023
VUS Results: Rates of Reclassification in Inherited Cancer Genes
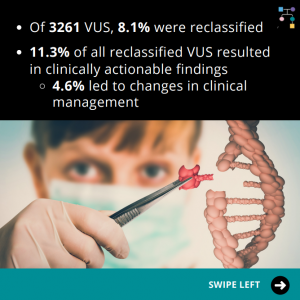
In a multicenter study evaluating reclassifications of variant of uncertain significance (VUS) results in breast, ovarian, and colorectal cancer susceptibility genes, it was discovered that of 3261 VUS results, 8.1% were reclassified. Of all the reclassified VUS results, 11.3% resulted in clinically actionable findings, and 4.6% led to changes in clinical management. The reclassification rates …
Permanent link to this article: https://inheritedcancer.net/post60523/
ICARE Featured Video November 2022
RAD51C Variants of Uncertain Significance
ICARE Featured Video November 2022
RAD51C Variants of Uncertain Significance
Below you may watch a featured video from the November 2022 Genetics Case Conference, which focused on RAD51C variants of uncertain significance with guest experts David Adams, PhD from the Wellcome Sanger Institute.
Permanent link to this article: https://inheritedcancer.net/video111022/
ICARE Featured Video June 2022
Updates on BRCA1 Variants of Uncertain Significance
ICARE Featured Video June 2022
Updates on BRCA1 Variants of Uncertain Significance
Below you may watch a featured video from the June 2022 Genetics Case Conference focused on updates on BRCA1 variants of uncertain significance with guest expert Alvaro Monteiro, PhD.
Permanent link to this article: https://inheritedcancer.net/video60222/
Permanent link to this article: https://inheritedcancer.net/post62221/
ICARE Social Media Post April 2021
Winter 2021 Ask the Expert
ICARE Social Media Post April 2021
Winter 2021 Ask the Expert
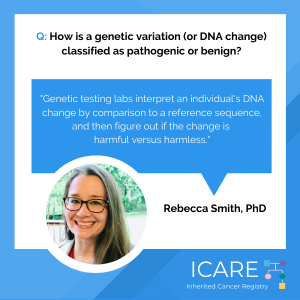
In every ICARE newsletter we give our participants the opportunity to have a question addressed by an expert in the field. In the latest edition, Dr. Rebecca Smith explains how a genetic change (or mutation) is classified as pathogenic or benign. Check out Dr. Smith’s full response in our Winter 2021 newsletter at: https://inheritedcancer.net/newsletters/
Permanent link to this article: https://inheritedcancer.net/post40921/
ICARE Newsletter Winter 2021
Ask the Expert
ICARE Newsletter Winter 2021
Ask the Expert
In each newsletter, we give participants the opportunity to have their questions addressed by experts in the field. This question was addressed by Rebecca Smith, PhD, Laboratory Director at Genetics Associates, Inc. with over 20 years of experience in biomedical research and 7 years of experience in clinical laboratory diagnostics. If you have a question …
Permanent link to this article: https://inheritedcancer.net/9nlw2021/
ICARE Social Media Post September 2020
NCCN Genetic Testing Choice Updates
ICARE Social Media Post September 2020
NCCN Genetic Testing Choice Updates
The National Comprehensive Cancer Network (NCCN) released new guidelines on September 8th, 2020, which included updates to genetic testing choices and considerations as follows: Choice of multi-gene panel may be guided by genes included, analyses offered, and financial assistance programs available for family testing Significant limitations in interpretations of polygenic risk scores: NOT recommended for …
Permanent link to this article: https://inheritedcancer.net/post91120/
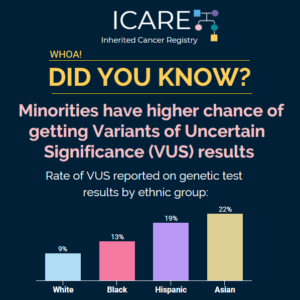
ICARE Social Media Post June 2020
Higher Chance of VUS Results in Minorities
ICARE Social Media Post June 2020
Higher Chance of VUS Results in Minorities
Asian, Hispanic, and Black women with breast cancer had higher rates of variants of uncertain significance (VUS) on genetic test results for hereditary cancer genes compared to White women with breast cancer according to a recent study. Check out the full article at https://link.springer.com/article/10.1007%2Fs13187-019-01646-8
Permanent link to this article: https://inheritedcancer.net/post62620/
ICARE Newsletter Winter 2019
Testing Interpretation and Variant Reclassification
ICARE Newsletter Winter 2019
Testing Interpretation and Variant Reclassification
Results of germline genetic testing generally yield three types of test results: Deleterious (positive), Negative (no mutation detected), and Variant of Uncertain Significance (VUS). As more genes are tested, the chance for a positive result goes up, as does the chance of receiving a VUS result.1 VUS results tell us that it remains uncertain whether …
Permanent link to this article: https://inheritedcancer.net/15nlw2019/
ICARE Newsletter Summer 2013
Sharing BRCA Test Results with Adolescent and Young Adult Children—What Does the Latest Research Show?
ICARE Newsletter Summer 2013
Sharing BRCA Test Results with Adolescent and Young Adult Children—What Does the Latest Research Show?
While there are specific recommendations against BRCA testing for minors,1 guidelines are less clear about whether parents should share their own test results with their children. Because there are no recommended surveillance or risk reduction options prior to age 25 for known BRCA mutation carriers, there has been debate about balancing the benefits of sharing …
Permanent link to this article: https://inheritedcancer.net/2nls2013/
ICARE Newsletter Summer 2011
Ask the Expert
ICARE Newsletter Summer 2011
Ask the Expert
We are fortunate to have Dr. Alvaro Monteiro, who is a molecular geneticist and expert on the BRCA1 and BRCA2 genes, as a member of our team. For our first ICARE newsletter, Dr. Monteiro teaches us about Variants of Uncertain Significance. Q. What is a Variant of Uncertain Significance (VUS) test result? How do researchers …
Permanent link to this article: https://inheritedcancer.net/1nls2011/