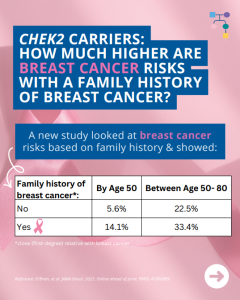
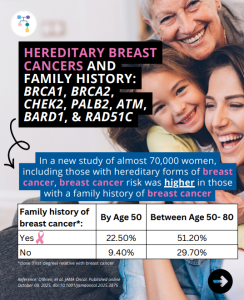
A new study looked at breast cancer risks in CHEK2 carriers based on family history and found that risks for breast cancer were much higher in those with a family history and additional non-genetic risk factors further modified risks. To learn more read the article at: https://jamanetwork.com/journals/jamaoncology/article-abstract/2839917 Reference: O’Brien, et al. JAMA Oncol. 2025. Online …
Gene: CHEK2
Permanent link to this article: https://inheritedcancer.net/post11192025/
Permanent link to this article: https://inheritedcancer.net/post10282025/
ICARE Newsletter Fall 2025
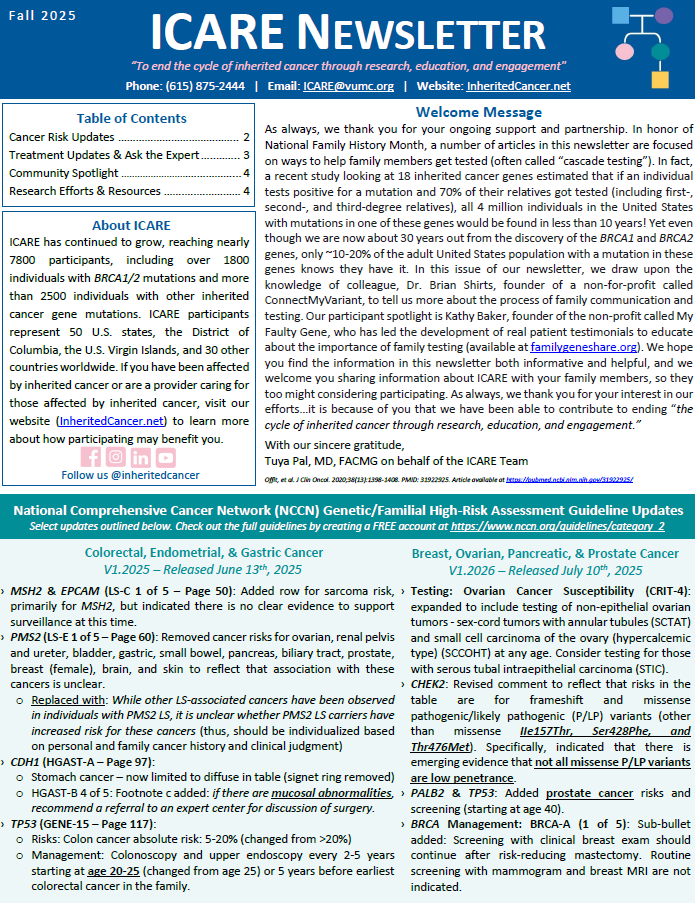
National Comprehensive Cancer Network (NCCN) Genetic/Familial High-Risk Assessment Guideline Updates
ICARE Newsletter Fall 2025
National Comprehensive Cancer Network (NCCN) Genetic/Familial High-Risk Assessment Guideline Updates
Select updates outlined below. Check out the full guidelines by creating a FREE account at https://www.nccn.org/guidelines/category_2 Colorectal, Endometrial, & Gastric Cancer V1.2025 – Released June 13th, 2025 Breast, Ovarian, Pancreatic, & Prostate Cancer V1.2026 – Released July 10th, 2025
Permanent link to this article: https://inheritedcancer.net/nlf20251/
ICARE Newsletter Fall 2025
ATM, CHEK2, & PALB2 Carriers: Are There Differences in Cancer-Associated Mortality?
ICARE Newsletter Fall 2025
ATM, CHEK2, & PALB2 Carriers: Are There Differences in Cancer-Associated Mortality?
A new study of ATM, CHEK2, and PALB2 carriers compared to non-carriers showed similar mortality from breast cancer, pancreatic cancer, and colorectal cancer. Other findings among BRCA1/2 carriers and Lynch Syndrome patients showed: 1) BRCA1/2 carriers had lower mortality from triple-negative breast cancer; and 2) Lynch Syndrome patients had lower mortality from colorectal cancer. Ultimately, …
Permanent link to this article: https://inheritedcancer.net/nlf20257/
ICARE Newsletter Fall 2025
Inherited Prostate Cancer: PARP Inhibitors
ICARE Newsletter Fall 2025
Inherited Prostate Cancer: PARP Inhibitors
A new study combined the results of prior studies of PARP inhibitors in patients with metastatic castration-resistant prostate cancer and an inherited gene mutation through a meta-analysis. The results showed that PARP inhibitors provided the greatest benefit in BRCA1/2 carriers and there was a strong signal of benefit in PALB2 or CDK12 alterations. However, there …
Permanent link to this article: https://inheritedcancer.net/nlf202510/
Permanent link to this article: https://inheritedcancer.net/post09092025/
ICARE Social Media Post August 2025
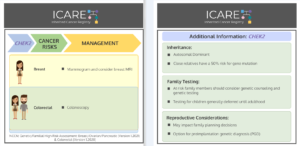
NCCN BOPP Guidelines (V1.2026): CHEK2
ICARE Social Media Post August 2025
NCCN BOPP Guidelines (V1.2026): CHEK2
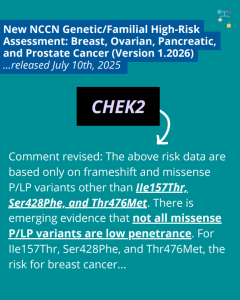
The National Comprehensive Cancer Network (NCCN) recently released updated Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate Cancer guidelines (Version 1.2026), which included updates to CHEK2 content. To learn more, check out the full guidelines by creating a FREE account at: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bopp.pdf
Permanent link to this article: https://inheritedcancer.net/post080825/
ICARE Social Media Post July 2025
NCCN Breast, Ovarian, Pancreatic, and Prostate Cancer Guidelines Update (V1.2026)
ICARE Social Media Post July 2025
NCCN Breast, Ovarian, Pancreatic, and Prostate Cancer Guidelines Update (V1.2026)
The National Comprehensive Cancer Network (NCCN) just released updated Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate Cancer guidelines (Version 1.2026) today! There are many updates found in these new guidelines including updates to CHEK2, PALB2, TP53, and PTEN content as well as BRCA cancer risk management and much more. To learn more, check out …
Permanent link to this article: https://inheritedcancer.net/post071025/
ICARE Social Media Post June 2025
ATM, CHEK2, & PALB2 Carriers: Are There Differences in Cancer-associated Mortality?
ICARE Social Media Post June 2025
ATM, CHEK2, & PALB2 Carriers: Are There Differences in Cancer-associated Mortality?
A new study showed that compared to non-carriers, ATM, CHEK2, and PALB2 carriers showed similar mortality from breast cancer, pancreatic cancer, and colorectal cancer. Other findings among BRCA1/2 carriers and Lynch Syndrome patients showed: Why is this important?These results may be reassuring for ATM, CHEK2, and PALB2 carriers, and provide additional useful information when discussing …
Permanent link to this article: https://inheritedcancer.net/post060625/
ICARE Social Media Post May 2025
Inherited Prostate Cancer: PARP Inhibitors
ICARE Social Media Post May 2025
Inherited Prostate Cancer: PARP Inhibitors
A new meta-analysis study looking at prior studies of PARP inhibitors in patients with metastatic castration-resistant prostate cancer and an inherited gene mutation showed: Learn more at: https://pubmed.ncbi.nlm.nih.gov/39848867/ Reference: Naqvi, et al. Eur Urol. 2025:S0302-2838(24)02760-X. PMID: 39848867.
Permanent link to this article: https://inheritedcancer.net/post52125/
ICARE Newsletter Spring 2025
Community Spotlight
ICARE Newsletter Spring 2025
Community Spotlight
As someone with two inherited cancer gene mutations—MSH6 (Lynch syndrome) and CHEK2 — I know firsthand the emotional and practical complexities of navigating hereditary cancer risk. My journey began without what many might consider “classic” red flags — just a few scattered cancer cases in my family, none of which seemed connected at the time. …
Permanent link to this article: https://inheritedcancer.net/12nls2025/
ICARE Newsletter Spring 2025
Refining Specific CHEK2 Mutation Risks
ICARE Newsletter Spring 2025
Refining Specific CHEK2 Mutation Risks
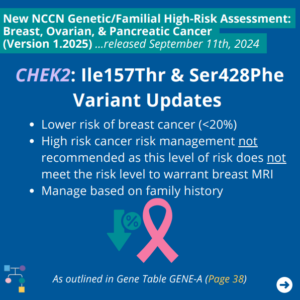
A recent editorial highlighted three common low-risk CHEK2 mutations (p.I157T, p.S428F, and p.T476M) that lead to a breast cancer risk of <1.4 fold (compared to “typical” CHEK2 mutations where the risk is over 2-fold).1 This is important because the level of risk for these mutations does not warrant high-risk screening. Another study on these three …
Permanent link to this article: https://inheritedcancer.net/8nls2025/
ICARE Social Media Post February 2025
CHEK2: Double Mutation Carriers and Risks
ICARE Social Media Post February 2025
CHEK2: Double Mutation Carriers and Risks
There are three CHEK2 “low-risk” mutations with lower breast cancer risks: p.I157T, p.S428F, and p.T476M. A new study was conducted on how combinations of low- and regular-risk CHEK2 mutations may affect breast cancer risk. Results showed the following risks for various combinations of variants: Accompanying editorial by Dr. Rajagopal highlights: Check out the articles to …
Permanent link to this article: https://inheritedcancer.net/post21025/
ICARE Social Media Post November 2024
Reduced Penetrance BRCA1/2 Pathogenic Variants
ICARE Social Media Post November 2024
Reduced Penetrance BRCA1/2 Pathogenic Variants
Check out our recently published study that brings attention to “reduced penetrance” BRCA1 and BRCA2 (BRCA) pathogenic variants, which impart LOWER breast cancer risks than ‘typical’ BRCA mutations. Specifically, lifetime breast cancer risks for these reduced penetrance BRCA variants are 20-30% which is similar to that seen in moderate penetrance breast cancer genes (e.g., CHEK2 …
Permanent link to this article: https://inheritedcancer.net/post111124/
ICARE Social Media Post October 2024
Personalized Screening Recommendations for CHEK2 Carriers
ICARE Social Media Post October 2024
Personalized Screening Recommendations for CHEK2 Carriers
A recent editorial highlights the value of personalized screening recommendations for CHEK2 carriers▪️ Notably, three common low-risk mutations (p.I157T, p.S428F, and p.T476M) impart a breast cancer risk of less than 1.4 fold▪️ This level of risk does not warrant high-risk breast screening or other heightened care Read the full article to learn more at: https://www.oncotarget.com/article/28604/pdf/ …
Permanent link to this article: https://inheritedcancer.net/post103124/
ICARE Social Media Post October 2024
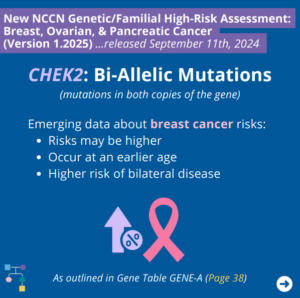
NCCN BOP Guideline Update #8: CHEK2 Bi-allelic Mutations
ICARE Social Media Post October 2024
NCCN BOP Guideline Update #8: CHEK2 Bi-allelic Mutations
The National Comprehensive Cancer Network (NCCN) released updated Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer guidelines on September 11th, 2024. In these updates, NCCN outlines emerging data regarding breast cancer risks for bi-allelic CHEK2 mutations (i.e., mutations in both copies of the gene) as outlined in GENE-A (Page 38) ⤸ To read more, you …
Permanent link to this article: https://inheritedcancer.net/post102424/
ICARE Social Media Post October 2024
NCCN BOP Guideline Update #7: CHEK2: Ile157Thr and Ser428Phe
ICARE Social Media Post October 2024
NCCN BOP Guideline Update #7: CHEK2: Ile157Thr and Ser428Phe
The National Comprehensive Cancer Network (NCCN) released updated Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer guidelines on September 11th, 2024. In these updates, NCCN outlines the following for the CHEK2 Ile157Thr and Ser428Phe variants as outlined in GENE-A (Page 38) ⤸ To read more, you can check out the full guidelines by creating a …
Permanent link to this article: https://inheritedcancer.net/post102324_1/
ICARE Social Media Post October 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 5
ICARE Social Media Post October 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 5
The National Comprehensive Cancer Network (NCCN) released the new Genetic/Familial High-Risk Assessment Colorectal, Endometrial, and Gastric Cancer guidelines on August 8th, 2024. An important update includes the revision of CHEK2 estimated absolute colon cancer risk to “NO INCREASED RISK”; thus, general population screening is appropriate for these individuals. You can check out the full guidelines …
Permanent link to this article: https://inheritedcancer.net/100624-2/
ICARE Newsletter Fall 2024
Risks of Cancer in Individuals with TWO CHEK2 Mutations (called “Bi-Allelic” Mutations)
ICARE Newsletter Fall 2024
Risks of Cancer in Individuals with TWO CHEK2 Mutations (called “Bi-Allelic” Mutations)
A new study found that risks may be higher for multiple types of cancer, including breast cancer, in both females and males who have two CHEK2 mutations: Additionally, findings showed that the type of mutation may be important to guide level of risk (e.g., truncating 1100delC homozygotes being at a higher risk than compound heterozygotes …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2024-risks-of-cancer-in-individuals-with-two-chek2-mutations-called-bi-allelic-mutations/
ICARE Newsletter Fall 2024
National Comprehensive Cancer Network (NCCN) Guideline Updates
ICARE Newsletter Fall 2024
National Comprehensive Cancer Network (NCCN) Guideline Updates
Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer – Released September 11th, 2024 (V1.2025) Check out the full guidelines by creating a FREE account at www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf Testing Updates: Gene Updates: Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, and Gastric Cancer – Released August 8th, 2024 (V1.2024) Check out the full guidelines by creating a FREE account at …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2024-national-comprehensive-cancer-network-nccn-guideline-updates/
ICARE Social Media Post September 2024
NCCN CEG Guideline Update #3: Use of HRT following premature surgical menopause
ICARE Social Media Post September 2024
NCCN CEG Guideline Update #3: Use of HRT following premature surgical menopause
The National Comprehensive Cancer Network (NCCN) released the new Genetic/Familial High-Risk Assessment Colorectal, Endometrial, and Gastric Cancer guidelines on August 8th, 2024. Updates include use of hormone replacement treatment following premature surgical menopause from risk-reducing oophorectomy. You can check out the full guidelines by creating a FREE account at:https://www.nccn.org/professionals/physician_gls/pdf/genetics_ceg.pdf
Permanent link to this article: https://inheritedcancer.net/poat92524/
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 3
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 3
The National Comprehensive Cancer Network (NCCN) released the new Genetic/Familial High-Risk Assessment Colorectal, Endometrial, and Gastric Cancer guidelines on August 8th, 2024. Updates include gynecologic risk and preventive surgery considerations for MLH1, MSH6, MSH2, and PMS2 carriers. You can check out the full guidelines by creating a FREE account at:https://www.nccn.org/professionals/physician_gls/pdf/genetics_ceg.pdf
Permanent link to this article: https://inheritedcancer.net/post91824/
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 2
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update – VERSION 2
The National Comprehensive Cancer Network (NCCN) released the new Genetic/Familial High-Risk Assessment Colorectal, Endometrial, and Gastric Cancer guidelines on August 8th, 2024. Updates include ⤸ You can check out the full guidelines by creating a FREE account at:https://www.nccn.org/professionals/physician_gls/pdf/genetics_ceg.pdf
Permanent link to this article: https://inheritedcancer.net/post91424/
ICARE Social Media Post September 2024
NCCN Breast, Ovarian, and Pancreatic Cancer Guidelines Update
ICARE Social Media Post September 2024
NCCN Breast, Ovarian, and Pancreatic Cancer Guidelines Update
The National Comprehensive Cancer Network (NCCN) released updated Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer guidelines on September 11th, 2024. Some updates include ⤸ To read more, you can check out the full guidelines by creating a FREE account at:https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf
Permanent link to this article: https://inheritedcancer.net/post91224/
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update
ICARE Social Media Post September 2024
NCCN Colorectal, Endometrial, and Gastric Cancer Guidelines Update
The National Comprehensive Cancer Network (NCCN) released the new Genetic Familial High-Risk Assessment Colorectal, Endometrial, and Gastric Cancer guidelines on August 8th, 2024. Updates include ⤸• Endometrial cancer recommendations included throughout• Hereditary Diffuse Gastric Cancer section added (HGAST-1)• Gynecologic risk and preventive surgery considerations for those with Lynch Syndrome• Use of hormone replacement treatment following …
Permanent link to this article: https://inheritedcancer.net/post90324/
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2024-new-guidelines-released-through-asco-society-of-oncology-germline-testing-in-patients-with-breast-center/
ICARE Newsletter Spring 2024
National Comprehensive Cancer Network (NCCN) Guideline Updates
ICARE Newsletter Spring 2024
National Comprehensive Cancer Network (NCCN) Guideline Updates
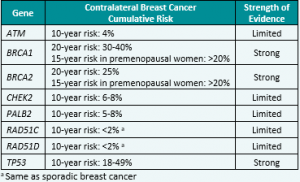
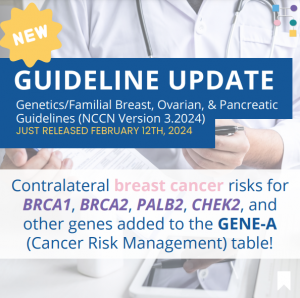
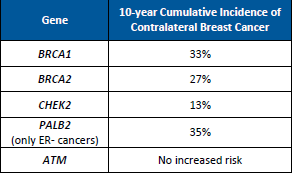
Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic Cancer – Released February 12th, 2024 (V3.2024) Check out the full guidelines by creating a FREE account at www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf Contralateral breast cancer risks in these updated guidelines: Expanded guidance about gynecologic cancers in BRCA1/2 carriers: Some highlights related to HRT include: Genetic/Familial High-Risk Assessment: Colorectal Cancer – Released …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2024-national-comprehensive-cancer-network-nccn-guideline-updates/
ICARE Social Media Post February 2024
Updates to NCCN Guidelines: Genetic/Familial Breast, Ovarian, and Pancreatic Post #1
ICARE Social Media Post February 2024
Updates to NCCN Guidelines: Genetic/Familial Breast, Ovarian, and Pancreatic Post #1
The National Comprehensive Cancer Network (NCCN) just released updated Genetic/Familial Breast, Ovarian, and Pancreatic Cancer guidelines on February 12th, 2024! Updates include adding contralateral breast cancer risks for BRCA1, BRCA2, PALB2, CHEK2, and other genes to the GENE-A (Cancer Risk Management) table 🧬 You can check out the full guidelines by creating a FREE account …
Permanent link to this article: https://inheritedcancer.net/post21324/
Permanent link to this article: https://inheritedcancer.net/post10524/
ICARE Featured Video October 2023
Management of Individuals with CHEK2 Mutations
ICARE Featured Video October 2023
Management of Individuals with CHEK2 Mutations
Below is a featured video from the October 2023 case conference, during which Helen Hanson, MD from the Royal Devon University Healthcare NHS Foundation Trust and Douglas Stewart, MD from the National Cancer Institute present on the management of individuals with CHEK2 germline pathogenic variants. Please visit our YouTube channel to watch the full October …
Permanent link to this article: https://inheritedcancer.net/video101223/
ICARE Newsletter Fall 2023
Newly released ACMG Clinical Practice Resource on CHEK2 Developed Through a Group of Worldwide Experts!
ICARE Newsletter Fall 2023
Newly released ACMG Clinical Practice Resource on CHEK2 Developed Through a Group of Worldwide Experts!
A person with a pathogenic variant in the CHEK2 gene may be at an increased risk for developing breast and other cancers. This ACMG Clinical Practice Resource, published in ACMG’s flagship journal, Genetics in Medicine, provides valuable information for healthcare providers caring for individuals with pathogenic variants in the CHEK2gene. This new ACMG Practice Resource …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2023-newly-released-acmg-clinical-practice-resource-on-chek2-developed-through-a-group-of-worldwide-experts/
ICARE Newsletter Fall 2023
National Comprehensive Cancer Network (NCCN) Guidelines Updates
ICARE Newsletter Fall 2023
National Comprehensive Cancer Network (NCCN) Guidelines Updates
Check out the full NCCN guidelines by creating a FREE account at www.nccn.org Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic CancerReleased August 28th, 2023 (V1.2024) › Transgender, Non-Binary, and Gender Diverse Individuals: NEW section on care (Page 63-66, TNBGD-1 to 4)› Li-Fraumeni Syndrome: Significant updates to content (risks and care) (Pages 57-60, LIFR-A): Table added …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2023-national-comprehensive-cancer-network-nccn-guidelines-updates/
Permanent link to this article: https://inheritedcancer.net/post100423/
ICARE Social Media Post August 2023
Updates to NCCN Guidelines: Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic
ICARE Social Media Post August 2023
Updates to NCCN Guidelines: Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic
The National Comprehensive Cancer Network (NCCN) just released updated Genetic/Familial Breast, Ovarian, and Pancreatic Cancer guidelines on August 28th, 2023, which included: You can check out the full guidelines by creating a FREE account at: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf
Permanent link to this article: https://inheritedcancer.net/post82923/
ICARE Social Media Post August 2023
New Article – Cancer Risk Management
ICARE Social Media Post August 2023
New Article – Cancer Risk Management
A recent study, which 𝗶𝗻𝗰𝗹𝘂𝗱𝗲𝗱 𝗜𝗖𝗔𝗥𝗘 𝗽𝗮𝗿𝘁𝗶𝗰𝗶𝗽𝗮𝗻𝘁𝘀, found that getting care according to guidelines depends on: Therefore, we need ways to improve knowledge among healthcare providers and trust in care among patients! Use this link to learn more: https://tinyurl.com/n26m4zys Reference: Dean, et al. Genet Med. 2023;100945. PMID: 37515473.
Permanent link to this article: https://inheritedcancer.net/post80723/
Permanent link to this article: https://inheritedcancer.net/post72623/
ICARE Social Media Post July 2023
Inherited Cancer Genes in Children: BRCA1/2, PALB2, ATM, CHEK2 , Lynch Genes
ICARE Social Media Post July 2023
Inherited Cancer Genes in Children: BRCA1/2, PALB2, ATM, CHEK2 , Lynch Genes
Recent study findings suggest that BRCA1/2, PALB2, ATM, CHEK2, and the Lynch Syndrome genes might confer reduced penetrance cancer risk among children. However, there are no adjustments to management or testing recommendations based on the level of risk (i.e., normally do not test children for conditions that primarily increase the risk of cancer in adulthood). …
Permanent link to this article: https://inheritedcancer.net/post72123/
ICARE Newsletter Spring 2023
Inherited Breast Cancer: Contralateral Breast Cancer Risks
ICARE Newsletter Spring 2023
Inherited Breast Cancer: Contralateral Breast Cancer Risks
While higher risks for contralateral breast cancer (CBC) have been known for BRCA1 and BRCA2, a newly published study demonstrated that the risk of CBC is also higher for female PALB2 and CHEK2 carriers; however, no elevated risks were found for ATM carriers (Table 1).1 This information is important to study, as it may be …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2023-inherited-breast-cancer-contralateral-breast-cancer-risks/
ICARE Social Media Post March 2023
BGREAT December 2022 Newsletter
ICARE Social Media Post March 2023
BGREAT December 2022 Newsletter
Check out the latest edition of our B-GREAT newsletter for updates about inherited cancers in the context of racial inequalities in healthcare. You can read the newsletter by visiting 👇https://bgreatinitiative.inheritedcancer.net/wp-content/uploads/BGREAT-December-2022-Newsletter.pdf Please feel free to share with family members, friends, and/or your healthcare providers.
Permanent link to this article: https://inheritedcancer.net/post30623/
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2022-ask-the-expert/
ICARE Newsletter Spring 2022
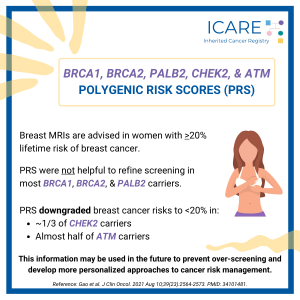
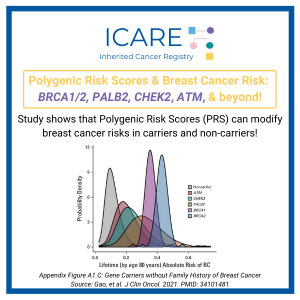
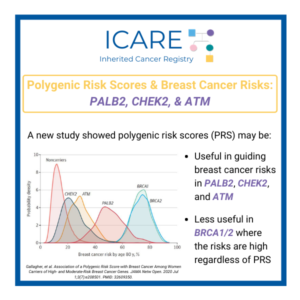
Polygenic Risk Scores and Inherited Breast Cancer Genes: BRCA1/2, PALB2, CHEK2, and ATM
ICARE Newsletter Spring 2022
Polygenic Risk Scores and Inherited Breast Cancer Genes: BRCA1/2, PALB2, CHEK2, and ATM
Breast MRIs are advised in women with >20% lifetime risk of breast cancer. A new study showed that breast cancer risks in BRCA1, BRCA2 and PALB2 carriers remained higher than 20%, regardless of whether polygenic risk scores (PRS) were done, suggesting this is of limited help in refining screening. In contrast, PRS downgraded breast cancer …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-spring-2022-polygenic-risk-scores-and-inherited-breast-cancer-genes-brca1-2-palb2-chek2-and-atm/
ICARE Newsletter Fall 2022
Screening & Treatment Updates: New Modeling Analysis About Breast Cancer Screening in ATM and CHEK2 Carriers
ICARE Newsletter Fall 2022
Screening & Treatment Updates: New Modeling Analysis About Breast Cancer Screening in ATM and CHEK2 Carriers
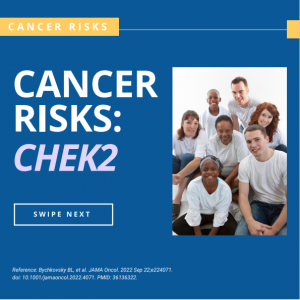
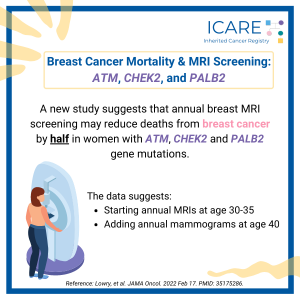
Using information from twelve prior population-based studies, a modeling analysis was done to look at when to start mammography and breast MRI in females with inherited mutations in genes including ATM and CHEK2. Overall, findings showed that starting annual MRI screening between age 30 to 35 and mammography at age 40 may lower death from …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2022-screening-treatment-updates-new-modeling-analysis-about-breast-cancer-screening-in-atm-and-chek2-carriers/
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2022-which-genes-are-confirmed-as-inherited-breast-cancer-genes/
ICARE Newsletter Fall 2022
Inherited Cancer Genes: New Associations
ICARE Newsletter Fall 2022
Inherited Cancer Genes: New Associations
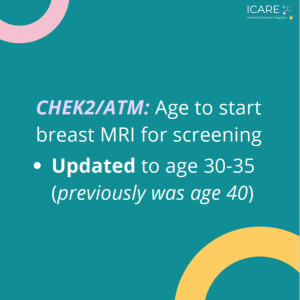
A new study led by colleagues at Vanderbilt University Medical Center, including our clinical geneticist colleague, Dr. Georgia Wiesner, evaluated 23 hereditary cancer genes and found 19 new gene associations including 7 new associations with cancer and 12 new associations with noncancer diseases. The associations with cancer versus other conditions is included in the table. …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2022-inherited-cancer-genes-new-associations/
ICARE Newsletter Fall 2022
National Comprehensive Cancer Network (NCCN) Guidelines Updates
ICARE Newsletter Fall 2022
National Comprehensive Cancer Network (NCCN) Guidelines Updates
Check out the full NCCN guidelines by creating a FREE account at www.nccn.org Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic – Released September 7th, 2022› Testing eligibility based on personal history of any type of breast cancer in females was updated from age ≤45 to ≤50 making more females with breast cancer eligible for testing …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2022-national-comprehensive-cancer-network-nccn-guidelines-updates/
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2021-ask-the-expert/
ICARE Newsletter Fall 2021
>
Polygenic Risk Scores and Breast Cancer Risks: BRCA1/2, PALB2, CHEK2, ATM , and beyond!
ICARE Newsletter Fall 2021
>Polygenic Risk Scores and Breast Cancer Risks: BRCA1/2, PALB2, CHEK2, ATM , and beyond!
A recent study found use of a polygenic risk score (PRS) modified the estimated riskof breast cancer among both carriers and non-carriers of inherited breast cancerpredisposition genes. Taking PRS into account, more than 95% of BRCA1, BRCA2,and PALB2 carriers had greater than 20% lifetime risks of breast cancer. In contrast,among ATM and CHEK2 carriers without …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-fall-2021-polygenic-risk-scores-and-breast-cancer-risks-brca1-2-palb2-chek2-atm-and-beyond/
Permanent link to this article: https://inheritedcancer.net/post40123/
ICARE Social Media Post December 2022
Bilateral Mastectomy in BRCA1/2, PALB2, ATM, & CHEK2 Carriers
ICARE Social Media Post December 2022
Bilateral Mastectomy in BRCA1/2, PALB2, ATM, & CHEK2 Carriers
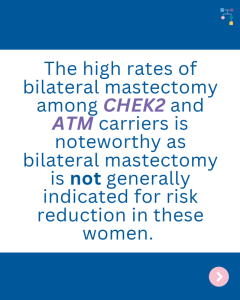
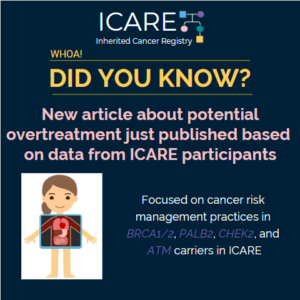
A recent study including data from ICARE participants found similar rates of bilateral mastectomy across high (BRCA1, BRCA2, PALB2) and moderate (ATM, CHEK2) penetrance genes. The high rates of bilateral mastectomies seen in those with moderate penetrance genes is concerning for overtreatment. Use the link to learn more: https://jamanetwork.com/journals/jamaoncology/fullarticle/2797978?guestAccessKey=fe9a3a20-8623-4feb-a0c5-315ad43a8fcb&utm_source=jps&utm_medium=email&utm_campaign=author_alert-jamanetwork&utm_content=author-author_engagement&utm_term=1m Reference: Reid et al. Receipt of …
Permanent link to this article: https://inheritedcancer.net/post120822/
Permanent link to this article: https://inheritedcancer.net/post112122-2/
ICARE Social Media Post October 2022
NCCN Familial/Genetic High Risk Assessment: Breast, Ovarian & Pancreatic Guidelines – single post 2
ICARE Social Media Post October 2022
NCCN Familial/Genetic High Risk Assessment: Breast, Ovarian & Pancreatic Guidelines – single post 2
On September 7th, 2022, the National Comprehensive Cancer Network (NCCN) released new breast, ovarian, and pancreatic cancer guidelines. In these new guidelines, the age to start breast MRI screening in female ATM and CHEK2 carriers was updated from age 40 to 30-35 making more females eligible for screening at an earlier age.Check out the new …
Permanent link to this article: https://inheritedcancer.net/post100222/
ICARE Social Media Post June 2022
New Variants Linked to Hereditary Cancer
ICARE Social Media Post June 2022
New Variants Linked to Hereditary Cancer
A new study evaluated 23 hereditary cancer genes and found 19 new gene associations, including 7 new associations with cancer and 12 new associations with non-neoplastic diseases. Specifically, the below genes were found to have an increased risk of disease:APC: benign liver/bile duct tumors, gastritis, and duodenitisATM: stomach cancer and pancreatic cancerBRCA1/2: ovarian cystsCHEK2: leukemia …
Permanent link to this article: https://inheritedcancer.net/post60122/
ICARE Social Media Post May 2022
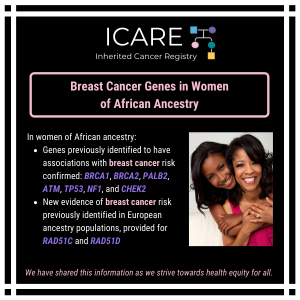
Breast Cancer Genes in Women of African Ancestry
ICARE Social Media Post May 2022
Breast Cancer Genes in Women of African Ancestry
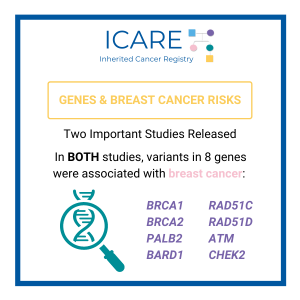
A recent study in women of African ancestry confirmed genes previously identified to have associations with breast cancer risk (BRCA1, BRCA2, PALB2, ATM, TP53, NF1, and CHEK2) and provided new evidence of breast cancer risk for RAD51C and RAD51D, which was identified previously in European ancestry populations.Check out the full article at 👇https://pubmed.ncbi.nlm.nih.gov/35396981/Reference: Díaz-Zabala, et …
Permanent link to this article: https://inheritedcancer.net/post51722/
ICARE Social Media Post April 2022
Breast Cancer Mortality & MRI Screening: ATM, CHEK2, and PALB2
ICARE Social Media Post April 2022
Breast Cancer Mortality & MRI Screening: ATM, CHEK2, and PALB2
A new study suggests that annual breast MRI screening may reduce deaths from breast cancer by half in women with ATM, CHEK2 and PALB2 gene mutations. The data suggests starting with annual breast MRIs between the ages of 30 to 35, and adding annual mammograms starting at age 40. Read the full article to learn …
Permanent link to this article: https://inheritedcancer.net/post40122/
Permanent link to this article: https://inheritedcancer.net/post20822/
Permanent link to this article: https://inheritedcancer.net/post20122/
Permanent link to this article: https://inheritedcancer.net/post82021/
Permanent link to this article: https://inheritedcancer.net/post81321/
Permanent link to this article: https://inheritedcancer.net/post62521/
Permanent link to this article: https://inheritedcancer.net/post40221/
Permanent link to this article: https://inheritedcancer.net/post30921/
Permanent link to this article: https://inheritedcancer.net/2nlw2021/
ICARE Newsletter Winter 2021
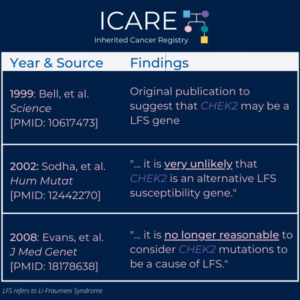
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
ICARE Newsletter Winter 2021
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
An old study back in 1999 suggested that CHEK2 may be a Li-Fraumeni Syndrome gene.1 However, a subsequent report in 2002 clearly refuted this original assertion, and based on additional data and analysis concluded that “… it is very unlikely that CHEK2 is an alternative Li-Fraumeni Syndrome susceptibility gene.”2 Another subsequent report in 2008 based …
Permanent link to this article: https://inheritedcancer.net/4nlw2021/
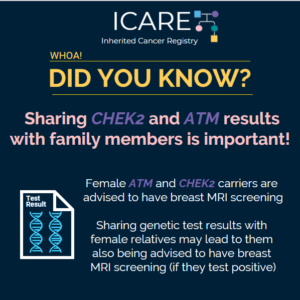
ICARE Social Media Post February 2021
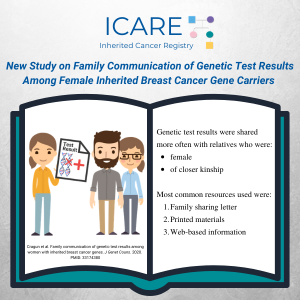
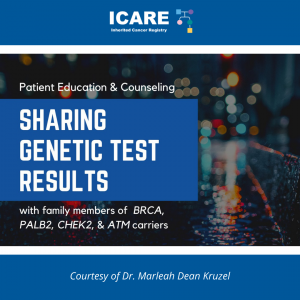
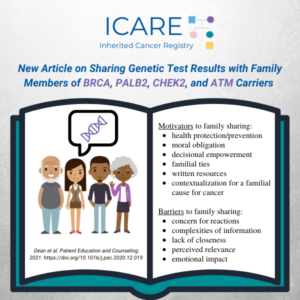
Sharing Genetic Test Results with Family Members of BRCA, PALB2, CHEK2, and ATM Carriers
ICARE Social Media Post February 2021
Sharing Genetic Test Results with Family Members of BRCA, PALB2, CHEK2, and ATM Carriers
Our team recently published “Sharing Genetic Test Results with Family Members of 𝘉𝘙𝘊𝘈, 𝘗𝘈𝘓𝘉2, 𝘊𝘏𝘌𝘒2, and 𝘈𝘛𝘔 Carriers” in 𝘗𝘢𝘵𝘪𝘦𝘯𝘵 𝘌𝘥𝘶𝘤𝘢𝘵𝘪𝘰𝘯 𝘢𝘯𝘥 𝘊𝘰𝘶𝘯𝘴𝘦𝘭𝘪𝘯𝘨 Special Issue on Genetics. View the article available at:https://www.sciencedirect.com/science/article/pii/S0738399120306832 Challenges and barriers to family sharing included concern for family members’ reactions, complexities of information, lack of closeness, perceived relevance, & emotional impact. …
Permanent link to this article: https://inheritedcancer.net/post20821/
ICARE Social Media Post January 2021
Sharing Genetic Test Results with Family Members of BRCA, PALB2, CHEK2, and ATM
ICARE Social Media Post January 2021
Sharing Genetic Test Results with Family Members of BRCA, PALB2, CHEK2, and ATM
Check out a new article by the ICARE team, published in Patient Education and Counseling, evaluating the motivators and barriers to sharing personal genetic test results with family members. The article is 𝗳𝗿𝗲𝗲 to access and download 𝘂𝗻𝘁𝗶𝗹 𝗠𝗮𝗿𝗰𝗵 𝟱𝘁𝗵 at: https://www.sciencedirect.com/science/article/pii/S0738399120306832
Permanent link to this article: https://inheritedcancer.net/post11521/
ICARE Publication January 2021
Sharing genetic test results with family members of BRCA, PALB2, CHEK2, and ATM carriers
ICARE Publication January 2021
Sharing genetic test results with family members of BRCA, PALB2, CHEK2, and ATM carriers
Abstract Objective: This study explored motivators and challenges/barriers to sharing personal genetic test results (GTR) with family members (FM). Methods: Semi-structured, in-depth interviews were conducted with 62 women who had a pathogenic or likely pathogenic (P/LP) variant in a BRCA, PALB2, CHEK2, or ATM gene. Selective qualitative data analysis focused on eliciting motivators and challenges/barriers …
Permanent link to this article: https://inheritedcancer.net/pub10521/
Permanent link to this article: https://inheritedcancer.net/post121820/
ICARE Featured Video November 2020
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
ICARE Featured Video November 2020
CHEK2 is NOT a Li-Fraumeni Syndrome Gene
Below you may watch a featured video from the November 2020 Genetics Case Conference, which outlined how CHEK2 is NOT a Li-Fraumeni Syndrome gene. For additional details, read the articles at the links below: 𝟭𝟵𝟵𝟵: https://pubmed.ncbi.nlm.nih.gov/10617473 𝟮𝟬𝟬𝟮: https://pubmed.ncbi.nlm.nih.gov/12442270 𝟮𝟬𝟬𝟴: https://pubmed.ncbi.nlm.nih.gov/18178638
Permanent link to this article: https://inheritedcancer.net/video111220/
ICARE Publication November 2020
Family communication of genetic test results among women with inherited breast cancer genes
ICARE Publication November 2020
Family communication of genetic test results among women with inherited breast cancer genes
Abstract Identification of inherited breast cancer may guide care. These benefits can be amplified through communication of genetic test results with at-risk family members and subsequent family testing (FT). Females with a pathogenic/likely pathogenic (P/LP) variant in BRCA1/2, PALB2, CHEK2, and/or ATM were surveyed about family communication (FC) of genetic test results and FT. Comparisons …
Permanent link to this article: https://inheritedcancer.net/pub111020/
Permanent link to this article: https://inheritedcancer.net/post102720/
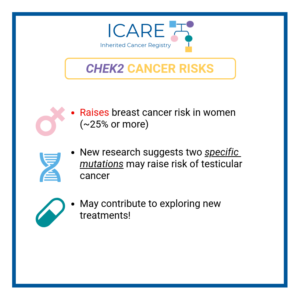
ICARE Social Media Post October 2020
CHEK2: Cancer Risks and Risk Management
ICARE Social Media Post October 2020
CHEK2: Cancer Risks and Risk Management
Gene: 𝘾𝙃𝙀𝙆2 Cancer Risks and Management per National Comprehensive Cancer Network (NCCN) Genetic/Familial High-Risk Assessment: Colorectal Version 1.2020 & Breast/Ovarian/Pancreatic Version 1.2021: 𝗪𝗼𝗺𝗲𝗻: Breast Cancer Risk: Elevated at 28-44% – Recommend annual mammogram starting at age 40 and consider annual breast MRIs with contrast starting at age 40. 𝗠𝗲𝗻 𝗮𝗻𝗱 𝗪𝗼𝗺𝗲𝗻: Colorectal Cancer Risk: Elevated …
Permanent link to this article: https://inheritedcancer.net/post100920/
Permanent link to this article: https://inheritedcancer.net/video100820/
ICARE Publication September 2020
Strategies to enhance identification of hereditary breast cancer gene carriers
ICARE Publication September 2020
Strategies to enhance identification of hereditary breast cancer gene carriers
No abstract available Reid S, et al. Strategies to enhance identification of hereditary breast cancer gene carriers. Expert Rev Mol Diagn. 2020 Sep; 20(9):861-865. Epub 2020 Sep 11. PMID: 32856489.
Permanent link to this article: https://inheritedcancer.net/pub91120/
ICARE Newsletter Summer 2020
Guideline-Concordant Care Among Women with Inherited Cancer Gene Mutations
ICARE Newsletter Summer 2020
Guideline-Concordant Care Among Women with Inherited Cancer Gene Mutations
Testing for inherited cancer among breast cancer patients has tremendous potential to guide appropriate care following testing. Yet, a number of efforts suggest that women are not consistently receiving care according to current national guidelines based on their genetic test result. In fact, results from studies suggest many women for whom risk-reducing mastectomy would not …
Permanent link to this article: https://inheritedcancer.net/3nls2020/
ICARE Social Media Post July 2020
Breast Cancer Risks May be Higher in Women with Two CHEK2 Mutations Versus One CHEK2 Mutation
ICARE Social Media Post July 2020
Breast Cancer Risks May be Higher in Women with Two CHEK2 Mutations Versus One CHEK2 Mutation
A study comparing women with two CHEK2 mutations to one CHEK2 mutation showed that those with two mutations were: -more likely to get breast cancer (80.6% versus 41.2%) -more likely to be diagnosed at or below age 50 (61.3% versus 23.9%) -more likely to have a second breast cancer diagnosis (22.6% versus 8.1%) These findings …
Permanent link to this article: https://inheritedcancer.net/post71720/
ICARE Social Media Post July 2020
BRCA1/2 and Other Gene Carriers with Breast Cancer Don’t Always Receive Recommended Treatment
ICARE Social Media Post July 2020
BRCA1/2 and Other Gene Carriers with Breast Cancer Don’t Always Receive Recommended Treatment
BRCA1/2 and other gene mutation carriers with early stage breast cancer are not always receiving cancer treatment as recommended by national guidelines. Even though more and more people have been tested for hereditary cancer over the years, using this information accurately to guide treatment has not been as successful. These findings highlight the need for …
Permanent link to this article: https://inheritedcancer.net/post71020/
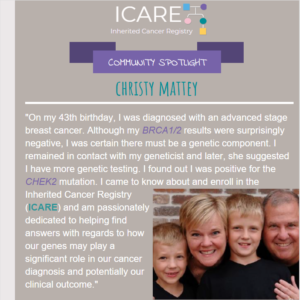
ICARE Social Media Post June 2020
Community Spotlight: Christy Mattey
ICARE Social Media Post June 2020
Community Spotlight: Christy Mattey
In every ICARE Newsletter we feature an ICARE participant as a community spotlight. Our latest community spotlight in our Winter 2017 ICARE Newsletter is Christy Mattey, who was found to have a CHEK2 mutation after a breast cancer diagnosis. Check out her story at: https://inheritedcancer.net/community-spotlight/
Permanent link to this article: https://inheritedcancer.net/post60920/
Permanent link to this article: https://inheritedcancer.net/post52920/
ICARE Social Media Post May 2020
Cancer Risk Management Among Female BRCA1/2, PALB2, CHEK2, and ATM Carriers in ICARE
ICARE Social Media Post May 2020
Cancer Risk Management Among Female BRCA1/2, PALB2, CHEK2, and ATM Carriers in ICARE
A new article was recently published based on data from BRCA1/2, PALB2, CHEK2, and ATM carriers in ICARE. Findings suggest potential overtreatment through risk-reducing surgery among women with pathogenic/likely pathogenic variants in breast cancer genes. This highlights the importance of promoting guideline-adherent, risk-appropriate care. Check out the full article at https://rdcu.be/b4mbg
Permanent link to this article: https://inheritedcancer.net/post52620/
ICARE Publication May 2020
Cancer risk management among female BRCA1/2, PALB2, CHEK2, and ATM carriers
ICARE Publication May 2020
Cancer risk management among female BRCA1/2, PALB2, CHEK2, and ATM carriers
Abstract Purpose: Identification of inherited breast cancer may guide cancer risk management. We sought to compare risk management practices across women with inherited breast cancer genes. Methods: Females with a pathogenic/likely pathogenic (P/LP) variant in BRCA1/2, PALB2, CHEK2, and/or ATM were surveyed about cancer risk management. Comparisons were made across genes. Results: The 235 participants with P/LP variants …
Permanent link to this article: https://inheritedcancer.net/pub52220/
ICARE Social Media Post March 2020
Study Based on ICARE Participants with ATM and CHEK2 Mutations
ICARE Social Media Post March 2020
Study Based on ICARE Participants with ATM and CHEK2 Mutations
Women with ATM and CHEK2 mutations have a lifetime breast cancer risk greater than 20%, which is the threshold at which screening through a breast MRI is recommended. A recently published study based on ICARE participants with ATM and CHEK2 mutations suggested that most female family members of ATM and CHEK2 mutation carriers do not …
Permanent link to this article: https://inheritedcancer.net/post32020/
ICARE Newsletter Winter 2020
New Study Based on ICARE Participants with ATM & CHEK2 Mutations
ICARE Newsletter Winter 2020
New Study Based on ICARE Participants with ATM & CHEK2 Mutations
We are excited to tell you about our recently published results based solely on data from ICARE participants with ATM and CHEK2 mutations. Our findings suggest most female family members of ATM and CHEK2 mutation carriers do not qualify for breast MRI screening based on family cancer history alone. This emphasizes the need to share …
Permanent link to this article: https://inheritedcancer.net/icare-newsletter-winter-2020new-study-based-on-icare-participants-with-atm-chek2-mutations/
ICARE Publication January 2020
Breast cancer screening implications of risk modeling among female relatives of ATM and CHEK2 carriers
ICARE Publication January 2020
Breast cancer screening implications of risk modeling among female relatives of ATM and CHEK2 carriers
Abstract Background: With the increasing use of multigene panel tests, pathogenic and likely pathogenic (P/LP) variants are identified more frequently in the moderate-penetrance breast cancer genes ATM and CHEK2. Lifetime breast cancer risk among women with P/LP variants in these genes generally exceeds 20%, meeting the threshold at which high-risk breast cancer screening through breast magnetic …
Permanent link to this article: https://inheritedcancer.net/pub12220/
ICARE Newsletter Summer 2019
New Information About Cancer Risks for Inherited Cancer Genes: CHEK2
ICARE Newsletter Summer 2019
New Information About Cancer Risks for Inherited Cancer Genes: CHEK2
In a study of inherited mutations in the CHEK2 gene, findings suggest there were two specific mutations that could predispose men to testicular germ cell tumors (TGCT). Specifically, 205 men with these tumors were tested for 48 DNA repair genes, and findings were then tested in other patient populations. These findings suggest that CHEK2 mutations …
Permanent link to this article: https://inheritedcancer.net/7nls2019/
ICARE Newsletter Winter 2019
New Online Risk Calculator to More Accurately Predict Breast Cancer Risk
ICARE Newsletter Winter 2019
New Online Risk Calculator to More Accurately Predict Breast Cancer Risk
Prediction of breast cancer risk is important to identify those at highest and lowest risks, to help guide screening. A previously developed risk algorithm called Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA) was recently extended to include truncating mutations in the BRCA genes, PALB2, CHEK2, and ATM. This online risk …
Permanent link to this article: https://inheritedcancer.net/11nlw2019/
ICARE Newsletter Summer 2018
New Data to Suggest Additional Genes Associated with Breast and Ovarian Cancer
ICARE Newsletter Summer 2018
New Data to Suggest Additional Genes Associated with Breast and Ovarian Cancer
A recent study reported on cancer risks among over 10,000 cancer patients across the United States who had genetic testing. Findings suggest breast cancer risks were associated with ATM, CHEK2, and PALB2, as expected; but an association was also found with MSH6 (in line with other recently published data, as outlined in another article in …
Permanent link to this article: https://inheritedcancer.net/7nls2018/
Permanent link to this article: https://inheritedcancer.net/2nls2017/
ICARE Newsletter Winter 2017
Community Spotlight
ICARE Newsletter Winter 2017
Community Spotlight
On my 43rd birthday I was diagnosed with an advanced stage breast cancer. Although my BRCA1 and BRCA2 results were surprisingly negative, I was certain there must be a genetic component to my breast cancer since I was diagnosed at a fairly young age. I remained in contact with my geneticist, Dr. Georgia Wiesner, and …
Permanent link to this article: https://inheritedcancer.net/spotlightnlw2017/
ICARE Newsletter Winter 2017
Characterizing Breast Cancers That Develop Among Women with a CHEK2 Mutation
ICARE Newsletter Winter 2017
Characterizing Breast Cancers That Develop Among Women with a CHEK2 Mutation
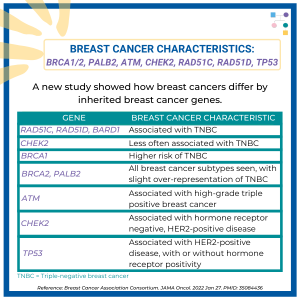
With increasing use of multi-gene panel tests, one of the genes in which mutations are frequently detected among breast cancer patients and others is the CHEK2 gene. This gene has been shown to have a 2-3 fold excess risk for breast cancer. There are many CHEK2 mutations that have been identified that generally fall into …
Permanent link to this article: https://inheritedcancer.net/8nlw2017/
ICARE Newsletter Winter 2017
NCCN Guidelines Version 1.2017: Genetic/Familial High-Risk Assessment: Breast and Ovarian
ICARE Newsletter Winter 2017
NCCN Guidelines Version 1.2017: Genetic/Familial High-Risk Assessment: Breast and Ovarian
Additional guidance pertaining to cancer risk management was provided in the most recent version of the NCCN Guidelines for inherited breast and ovarian cancer. These guidelines now include an expanded table outlining cancer risks and management for each gene, taking into account the age at initiation of each risk management modality as well as footnotes …
Permanent link to this article: https://inheritedcancer.net/1nlw2017/
ICARE Newsletter Summer 2016
CHEK2 *1100delC Mutation Carriers: Breast Cancer Risk by Age and Tumor Type and Other Associated Cancer Risks
ICARE Newsletter Summer 2016
CHEK2 *1100delC Mutation Carriers: Breast Cancer Risk by Age and Tumor Type and Other Associated Cancer Risks
The CHEK2 *1100delC mutation is the most common “truncating” mutation (causing a shortened protein) in the CHEK2 gene among Europeans, with lifetime breast cancer risk in the range of 20-30% among female carriers. Results of data pooled from over 30 studies which included 40,000 breast cancer cases and 40,000 controls, showed that estrogen receptor (ER) …
Permanent link to this article: https://inheritedcancer.net/6nls2016/
ICARE Newsletter Summer 2016
Practice Guideline Updates for NCCN Genetic/Familial High-Risk Assessment
ICARE Newsletter Summer 2016
Practice Guideline Updates for NCCN Genetic/Familial High-Risk Assessment
The National Comprehensive Cancer Network (NCCN) is a network of oncology healthcare providers who work together to develop best practice guidelines for the delivery of cancer care. Given the increasing use of testing for mutations in several inherited cancer genes at one time (called “multi-gene panel testing”), the Breast/Ovarian and Colorectal Panels sought to provide …
Permanent link to this article: https://inheritedcancer.net/2nls2016/
ICARE Newsletter Summer 2016
An Approach to Making Risk Management Recommendations for Newer Inherited Cancer Genes
ICARE Newsletter Summer 2016
An Approach to Making Risk Management Recommendations for Newer Inherited Cancer Genes
A recent article sought to develop an approach to cancer risk management among individuals with mutations in newer inherited cancer genes, many of which result in a moderate (rather than ‘high’) cancer risk. Overall, the investigators suggest a framework that takes the age-specific, lifetime, and absolute cancer risks into account for inherited cancer genes where …
Permanent link to this article: https://inheritedcancer.net/3nls2016/
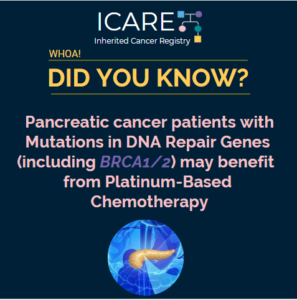
ICARE Newsletter Winter 2016
Potential Use of PARP-Inhibitors Among Men with Prostate Cancer Who Carry a Mutation in BRCA or Other DNA-Repair Gene
ICARE Newsletter Winter 2016
Potential Use of PARP-Inhibitors Among Men with Prostate Cancer Who Carry a Mutation in BRCA or Other DNA-Repair Gene
A recent study published in the New England Journal of Medicine suggests that PARP-Inhibitors may be of potential use in men who are no longer responding to standard treatments and carry either somatic (i.e., tumor) and/or germline (inherited) mutations in DNA-repair genes (i.e., BRCA1/2, ATM, Fanconi Anemia genes and CHEK2).1 Of 49 men with prostate …
Permanent link to this article: https://inheritedcancer.net/4nlw2016/
Permanent link to this article: https://inheritedcancer.net/1nls2015/